
Source: PublicDomainPictures via Wikimedia Commons.
The first time I learned PCR in the lab, it felt like unlocking a master key. Need to clone a gene? PCR. Want to sequence DNA? PCR. Trying to detect whether a virus is hiding inside a cell? PCR again. It quickly became clear that this single technique sits at the center of modern biology.
Years later, I realized PCR doesn’t just live in research labs. It follows us into clinics and hospitals too. When we feel sick and a doctor orders a virus test, PCR is often the tool used to look for infection.
But PCR isn’t the only way to detect a virus. Rapid antigen tests now sit on pharmacy shelves and in home medicine cabinets, offering a faster, though different, approach.
Both tests try to answer the same question: is a virus present?
The difference is how they do it, and that difference determines when each test works best.
How PCR Tests Work
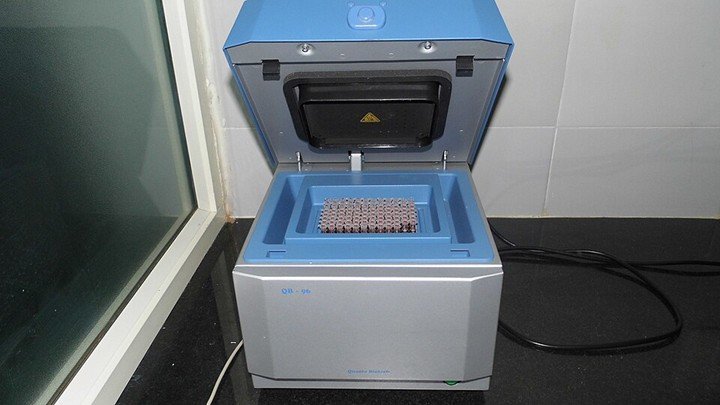
PCR thermocycler. Source: Microrao via Wikimedia Commons.
PCR stands for Polymerase Chain Reaction. This lab method looks for genetic material of a virus, which is usually RNA. That’s why a nose or throat swab is being used to collect the sample in PCR tests. Here are the basic steps associated with the PCR test.
- First, the lab will extract genetic material from your sample.
- Then a specialized enzyme will copy viral RNA after converting it into DNA.
- The machine cycles through heating and cooling steps that doubles DNA over and over.
- With each cycle, the amount of viral genetic materials will grow.
If the virus is present, PCR can amplify it, so that it is easily detected. That’s why PCR tests are quite popular for their high sensitivity tests. It can even pick trace amounts of virus.
How Antigen Tests Work
Antigen tests look for pieces of viral proteins instead of their genetic material. As a result, this is often a rapid test that can be done on a card or a strip. In other words, antigen tests are more similar to at home pregnancy tests. Here’s how it works:
- You swab your nose and mix the sample in a small liquid buffer.
- That liquid will flow along a test strip.
- If viral proteins are present, they bind antibodies into the strip.
- A colored line will appear when the virus is detected.
Which Test is More Accurate?
If you focus on pure detection power, PCR test is more sensitive when compared to antigen. That’s because it can detect smaller amounts of virus and is less likely to miss infections. That’s the same reason why doctors and hospitals consider PCR as the Gold Standard in many virus tests.
However, antigen tests have their own benefits. They tend to be positive when the viral load is high. As a result, you can use an antigen test to determine whether it is possible for a person to be infectious to others. On the other hand, antigen tests are quite effective when making real time decisions.
You can think of it like this. PCR is a microscope that sees the smallest trace. However, antigen test is more like a bright warning light that turns on when the virus is present at higher levels.
The Takeaway
PCR may have started for me as a lab technique, but its real-world impact goes far beyond research benches. In clinical care, PCR tests remain the most sensitive way to detect viral infections and confirm a diagnosis when symptoms appear.
Antigen tests, however, serve a different role. They provide rapid answers that help guide everyday decisions, whether someone should stay home, return to work, or avoid exposing others. Because they detect higher viral loads, they can be especially useful for identifying people who may be contagious.
A negative antigen result doesn’t always rule out infection. When symptoms persist, a follow-up PCR test offers the clearest confirmation. For public-health screening, repeated antigen testing can still be powerful, since it is fast, affordable, and easy to repeat over time.
From the lab bench to the clinic to the pharmacy shelf, both tools help answer the same question: is a virus present, and what should we do next?
