
San Juan, Puerto Rico. Source: Güldem Üstün via Wikimedia Commons.
Highlights
- A Major Age Shift in Dengue Cases
- DENV-3 Now Dominates Transmission
- Hospitalizations Exceed 50%
- A Regional Warning Signal
The 2026 Super Bowl reminded us of the power of discipline and consistency, qualities embodied by the players on the field.
But it also showcased something deeper: the strength of diversity in the United States, where Hispanic and Latino communities make up nearly 19% of the population. Representation matters. Culture matters. And this year, Puerto Rico stood at the center of that conversation.
When Bad Bunny performed and echoed the message of “El Apagón,” he spotlighted the island’s ongoing electrical instability and infrastructure challenges.
But the phrase “Puerto Rico está bien cabrón” captures more than political frustration or economic strain. It reflects resilience, and it also reflects struggle. Beyond infrastructure collapse and energy crises, Puerto Rico continues to battle a persistent biological threat: dengue virus.
While cultural moments grab headlines, pathogens move quietly.
A recent CDC report by Rodriguez et al. published in MMWR analyzed dengue cases reported to the Puerto Rico Department of Health from January 2010 through November 4, 2024. The findings go beyond routine surveillance updates. They reveal structural shifts in who is getting infected, which viral strains dominate, and how severe the disease has become.
So what can public health officials learn from this report? And what should the broader community understand?
This article breaks down the key epidemiologic findings and what they mean for dengue control, surveillance strategy, and public awareness in Puerto Rico and across Latin America.
Rising Adult Cases and a Major Age Shift in the 2023–2024 Outbreak

Afro-Puerto Rican women in Bomba dance attair. Source: Spreadofknowledge via Wikimedia Commons.
The analysis of dengue cases reported to the Puerto Rico Department of Health from 2010 through November 2024, encompassing 39,094 confirmed cases, reveals clear epidemiologic transitions when comparing three surveillance periods: 2010–2019, 2020–2022, and 2023–2024.
The most striking change is the shift in patient age.
During 2010–2019, the median age of dengue patients was 19 years. It declined slightly to 17 years during 2020–2022. But in 2023–2024, the median age increased sharply to 26 years. Nearly two-thirds of recent cases occurred in adults aged 20 years or older.
This is not merely a reflection of population aging. Incidence per 100,000 population increased substantially among adults aged 20–39 and those aged 40 and older.
In other words, dengue is now infecting adults at higher rates than in previous outbreak cycles.
The likely explanation lies in shifting immunity landscapes. After intense transmission in the early 2010s, fewer infections occurred in subsequent years. Adults who were previously protected may now face waning or incomplete immunity, leaving them more susceptible when new serotypes emerge.
DENV-3 Replaces DENV-1 in the 2023–2024 Outbreak
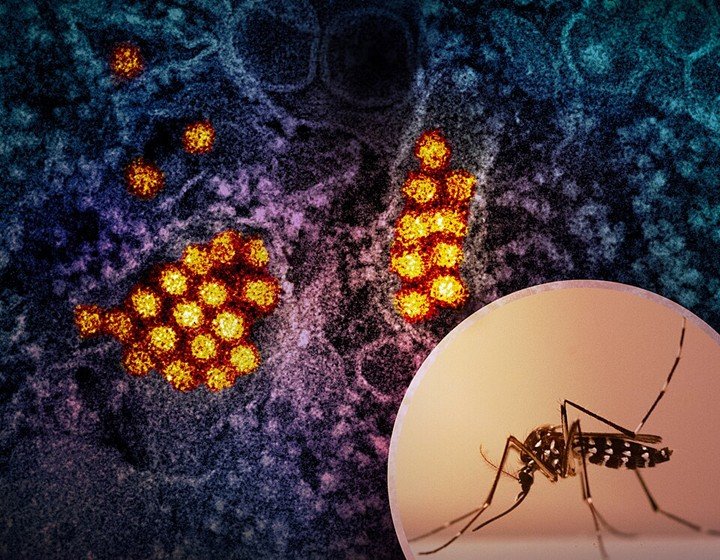
Dengue virus and Aedes mosquito. Source: NIAID via Wikimedia Commons.
For more than a decade, DENV-1 dominated circulation in Puerto Rico. Between 2010 and 2019, it accounted for over 70% of identified infections. Even during the early 2020–2022 resurgence, DENV-1 represented more than 90% of typed cases.
However, during 2023–2024, that dominance collapsed. DENV-3 became the predominant serotype, accounting for nearly 46% of cases, while DENV-2 also increased substantially. DENV-1 declined to just over one-third of infections, and DENV-4 virtually disappeared.
This serotype replacement matters. Infection with one dengue serotype provides long-term immunity against that specific strain but only transient protection against others. When a previously uncommon serotype reenters circulation in a partially immune population, susceptibility increases.
Moreover, secondary infection with a different serotype elevates the risk of severe disease through immune-mediated mechanisms. DENV-2 and DENV-3, in particular, have been associated with higher rates of severe illness and hospitalization compared to DENV-1.
DENV-3 and Older Adults Drive Increased Severity
Source: Pixnio.
Hospitalization data from 2023–2024 confirm this concern. During 2010–2019, approximately 36% of reported dengue cases required hospitalization. That proportion increased modestly during 2020–2022. In the current outbreak, however, 53.5% of reported patients were hospitalized. More than half of confirmed cases required inpatient care.
Hospitalization was highest among patients infected with DENV-3, followed by DENV-2.
Older adults also experienced marked increases in hospitalization compared to previous outbreak periods. Adults aged 40 years and older saw hospitalization rates exceed 50% during 2023–2024.
Despite this increase in severity indicators, fatality rates remained low and stable at approximately 0.2–0.3%, suggesting that early diagnosis and supportive care continue to prevent most deaths.
Several factors likely contribute to rising hospitalization rates. The emergence of DENV-3 and DENV-2 into a population with limited recent exposure increases the likelihood of secondary infections and more severe clinical presentations.
Longer intervals between infections have also been associated with greater disease severity. Additionally, older adults may carry comorbidities that heighten vulnerability to complications. Expanded surveillance and broader testing capacity in recent years may also capture more hospitalized cases than in prior cycles, improving ascertainment.
What This Means for Dengue Surveillance and Preparedness

Source: USDA by Preston Keres via Flickr.
Taken together, these findings describe a structural shift in dengue epidemiology in Puerto Rico. The virus is circulating differently. The population at risk has expanded. Clinical burden has intensified.
For public health systems, these changes carry important implications. Clinicians should recognize that dengue is no longer primarily an adolescent disease. Adult patients, including those with underlying conditions, now represent a substantial proportion of severe cases.
- Hospitals should anticipate the possibility of higher admission rates during transmission peaks.
- Surveillance programs would benefit from continuing detailed serotype monitoring to detect and respond to future replacement events early.
- Public communication campaigns should emphasize that adults remain at significant risk and encourage early care-seeking when febrile illness develops.
Puerto Rico’s experience may also serve as a warning signal for neighboring regions.
Similar DENV-3 resurgences have contributed to outbreaks in Brazil, Cuba, and Mexico in recent years. As immunity patterns shift across Latin America, other countries may encounter comparable changes in age distribution and hospitalization burden.
Dengue is not static. Its epidemiology evolves with changing immunity, serotype cycling, vector dynamics, and demographic shifts. The current outbreak in Puerto Rico illustrates how quickly those changes can reshape clinical and public health realities.
At Pathogenos, we see these data as more than surveillance trends. They offer an opportunity for anticipatory action. By understanding who is getting infected, which serotypes dominate, and how severity patterns shift, health systems can adapt proactively, before capacity becomes strained.
Dengue appears to have entered a new phase in Puerto Rico. Public health strategies should evolve alongside it.




