
Figure 1. CDC Gravid Trap for mosquito surveillance and pathogen testing. Source: NIAID, Flickr.
In 2024, Latin America and the Caribbean faced the worst dengue outbreak in recorded history, with over 12.6 million suspected cases and more than 7,700 deaths, according to a recent Reuters report.
The crisis has escalated into a major public health emergency, with countries like Brazil, Argentina, Colombia, and Mexico accounting for nearly 90% of reported cases and 88% of dengue-related deaths. What is even more alarming is that children under 15 made up a significant portion of severe cases.
So why are surveillance programs so critical in the fight against dengue in Latin America? In this blog, we break down the current outbreak, highlight what’s working, and explore how regional and national surveillance efforts are helping detect outbreaks early, inform public health responses, and ultimately save lives.
Climate and Urbanization Drive Aedes Aegypti Spread, Urging Stronger Dengue Surveillance
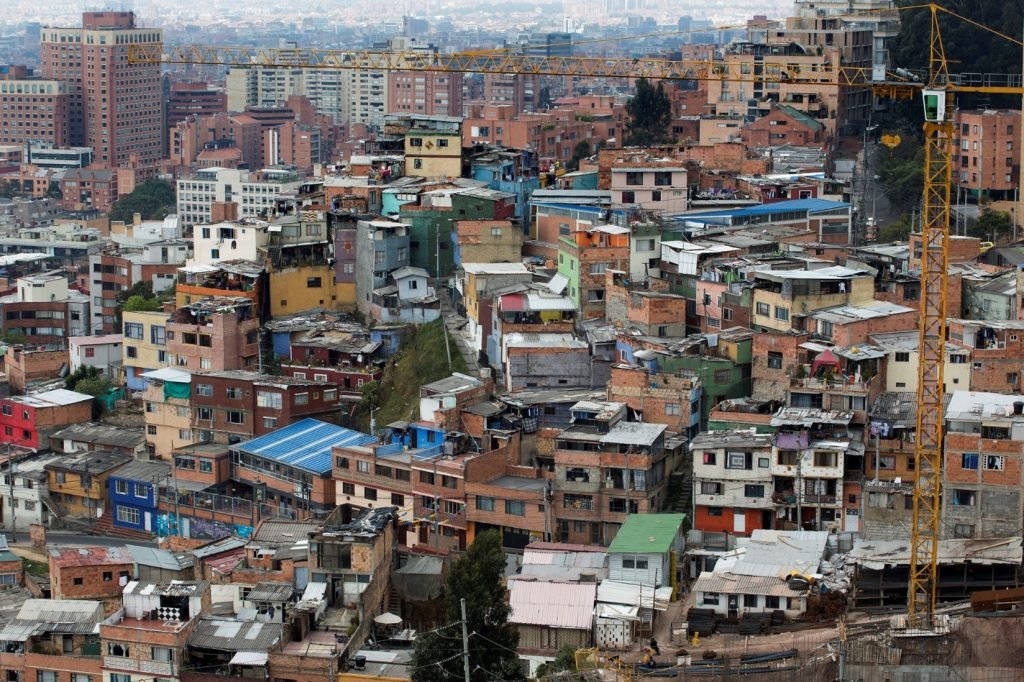
Figure 2. Citiview of Bogotá, Colombia. Source: World Bank Photo Collection via Flickr.
Scientists attribute the explosive growth of dengue cases to a perfect storm of factors: climate change and increased rainfall, rapid urbanization with overcrowded housing, and poor sanitation and ineffective waste management
These conditions create ideal breeding grounds for the Aedes aegypti mosquito, the primary vector of dengue, Zika, and chikungunya viruses. Unlike other mosquitoes, Aedes aegypti prefers to lay eggs in small, stagnant water containers found in homes, like flower pots, water tanks, and discarded tires. Worse yet, they bite during the daytime, rendering traditional bed nets useless.
In a recent gathering hosted by the University of Miami’s Institute for Advanced Study of the Americas, leading public health experts addressed the unprecedented 2024 dengue crisis in Latin America and the Caribbean. Experts linked the surge in dengue fever to several critical factors, including climate change, urban overcrowding, increased human mobility, and inadequate mosquito control infrastructure.
During the webinar, health experts called for stronger dengue surveillance systems, better public health infrastructure, and community-led mosquito control. They also stressed the need for regional collaboration and fair access to dengue vaccines like Qdenga® (TAK-003).
Dengue Vaccines Exist but Remain Less Accessible Than Mosquito Control

Figure 3. Photo of the Qdenga vaccine taken at the Policlínica Maria Tadeu de Aguiar in Santana, Brazil. Santana/AP. Source: Ministério da Saúde via Flickr.
Although Qdenga® (TAK-003), a dengue vaccine developed by Takeda, has been approved in countries like Brazil, Peru, and Argentina, it is still not widely available across Latin America.
In May 2024, the World Health Organization (WHO) prequalified the vaccine, making it eligible for international procurement through organizations like UNICEF and the Pan American Health Organization (PAHO). Yet, most countries have not added it to their national immunization programs due to several challenges:
Limited availability and high cost: In Argentina, the vaccine costs about 70,000 pesos (~$70 USD), which is significant given that the minimum monthly wage is around $200 USD.
Cold-chain storage issues: The vaccine must be stored at controlled temperatures, which is difficult in remote or under-resourced areas.
Complex rollout logistics: Large-scale vaccination campaigns require strong infrastructure, planning, and workforce, which many regions currently lack.
To address supply issues, Takeda has partnered with Biological E to increase production to 100 million doses per year by the end of the decade. However, these efforts are still in progress, and widespread access remains limited.
Other vaccines, like Dengvaxia®, come with restrictions. It is only recommended for people who have already had dengue, as studies show it may increase the risk of severe illness in individuals without prior exposure. This makes pre-vaccination testing necessary, complicating public health rollout and slowing adoption.
As a result, mosquito surveillance and vector control continue to be the frontline defense against dengue in Latin America. Until vaccines become more affordable and easier to distribute, environmental cleanup, larval control, and community awareness campaigns remain the most effective tools for preventing outbreaks.
Mosquito Surveillance Help Protect Latino Communities from Dengue
In a recent study by Mojica et al. published in the Journal of Medical Entomology, researchers monitored Aedes aegypti mosquitoes in two dengue-endemic countries: Nicaragua and Ecuador.
Over the course of one year, entomological surveillance teams visited more than 2,800 randomly selected households across eight communities (two in Nicaragua and six in Ecuador), as well as 100 public sites in Nicaragua.
Using backpack aspirators, which are handheld vacuum devices designed to safely collect adult mosquitoes, scientists captured female Aedes aegypti mosquitoes directly from homes and surrounding areas.
This real-world collection method provided critical insights into the mosquito populations most likely to transmit arboviruses in human environments.
Molecular Testing Reveals Active Dengue Circulation During Peak Season

Figure 4. Preventing Dengue Fever Story and photos by Chris Aguinaldo, Naval Region Hawaii Public Affairs. Source: Navy Medicine via Flickr.
After collecting the mosquitoes, scientists grouped them into 1,358 small sample sets, kind of like putting them into labeled test tubes. From each group, they looked for traces of the dengue virus by testing the mosquito’s genetic material using a highly accurate lab technique called real-time RT-PCR. This test is very sensitive and is often called the “gold standard” because it is one of the best ways to detect viruses.
The results showed that 10 of the mosquito groups (three from Nicaragua and seven from Ecuador) had dengue virus in them. All of these positive results happened during the rainy season, which is when mosquito-borne diseases like dengue are most likely to spread.
Importantly, the dengue virus serotypes identified in mosquitoes matched those reported in human dengue cases from the same regions. This confirms that entomological surveillance can act as a reliable early warning system for dengue outbreaks.
The study highlights how mosquito-based surveillance is a cost-effective, scalable strategy to improve public health preparedness and dengue control in Latin America and other endemic regions.
Some Mosquito Surveillance Strategies Fall Short
To better understand which dengue prevention strategies are most effective in Latin America and the Caribbean, Leandro and Maciel-de-Freitas et al. conducted a large-scale scoping review on Aedes mosquito control.
Published in JMIR Public Health and Surveillance, the study examined evidence from 2000 to 2021, drawing data from leading scientific databases such as MEDLINE, Scopus, EMBASE, and the Cochrane Library, along with reports from governments and NGOs.
The research team screened hundreds of studies using the Rayyan platform to ensure only high-quality, relevant findings were included. In total, they reviewed 122 studies testing mosquito control strategies in real-world settings, with a focus on Aedes aegypti.
Integrated Approaches Show the Most Promise in Dengue Control
The review found that the most effective mosquito control programs were those that combined several methods.
Strategies such as deploying biological control agents (like larvae-eating fish or bacteria), improving environmental sanitation, and boosting community engagement and education proved especially powerful in reducing mosquito populations, larval breeding, and even infection rates.
However, the study also highlighted major challenges. Many programs faced issues such as inconsistent funding, shortages of trained personnel, and poor coordination between health, environmental, and municipal sectors. These gaps often limited the long-term impact of mosquito control efforts.
By identifying both the successes and shortcomings of past interventions, this review offers a clear roadmap for future dengue control strategies in Latin America.
It underscores the need for integrated, community-driven, and well-funded approaches to sustainably manage Aedes-borne diseases across the region.
Latin America Implements Several Mosquito Surveillance Strategies

Figure 5. Vector surveillance. Ilma Marquez attempts to trap mosquitos for removal and further study in San Pedro Sula, Honduras, as part of Continuing Promise 22. Source: Navy Medicine via Flickr.
Latin America has implemented a multi-tiered dengue surveillance system to combat the growing threat of Aedes aegypti-borne diseases such as dengue, Zika, and chikungunya. This system integrates regional coordination, national disease tracking, and laboratory diagnostics to improve early detection and public health responses.
At the regional level, the Pan American Health Organization (PAHO) and World Health Organization (WHO) operate the Health Information Platform for the Americas (PLISA). This platform compiles weekly reports from member countries on dengue cases, deaths, mosquito distribution, and circulating serotypes. By enabling real-time outbreak monitoring, PLISA supports rapid public health action and guides decisions on vaccine deployment, resource allocation, and emergency interventions.
Nationally, countries have developed customized mosquito surveillance strategies. Brazil uses the SINAN system to track reportable diseases, while LIRAa conducts larval index surveys to identify Aedes aegypti breeding hotspots and direct targeted mosquito control.
In Colombia, the SIVIGILA system monitors suspected and confirmed dengue cases, hospitalizations, and serotype circulation, enabling coordination with the National Institute of Health and PAHO. Mexico’s SISVER system integrates virological, entomological, and clinical data to monitor dengue, Zika, and chikungunya outbreaks in real time.
To reinforce these national systems, Latin America relies on laboratory networks and digital surveillance tools. The Red de Laboratorios de Diagnóstico de Arbovirus (RELDA), supported by PAHO, the CDC, and national health institutions, improves diagnostic capacity by tracking dengue serotypes and monitoring genetic changes in the virus. This lab-based surveillance is essential for identifying emerging strains and anticipating severe outbreaks.
Global platforms like HealthMap, ProMED, and GIDEON complement local systems by aggregating real-time outbreak reports from ministries of health, news outlets, and public databases. These tools help forecast transmission trends and alert authorities to dengue hotspots before case numbers surge.
Together, these multi-layered mosquito surveillance strategies form the backbone of dengue control in Latin America, supporting faster responses, targeted interventions, and improved regional preparedness against arboviral diseases.
Mosquito Surveillance and Control Are Our Strongest Defense Against Dengue
With dengue cases surging, children at risk, and climate conditions favoring mosquito growth, disease surveillance is more critical than ever. From neighborhood mosquito sweeps to cutting-edge molecular diagnostics, Latin America’s public health leaders are investing in tools that protect lives.
But for these efforts to succeed, governments, scientists, and communities must work together. Surveillance is not just data collection. It is the foundation of proactive, life-saving action in the fight against dengue and other arboviral threats.





