Figure 1. Antibiotic drugs. Source: Global Panorama via Flickr.
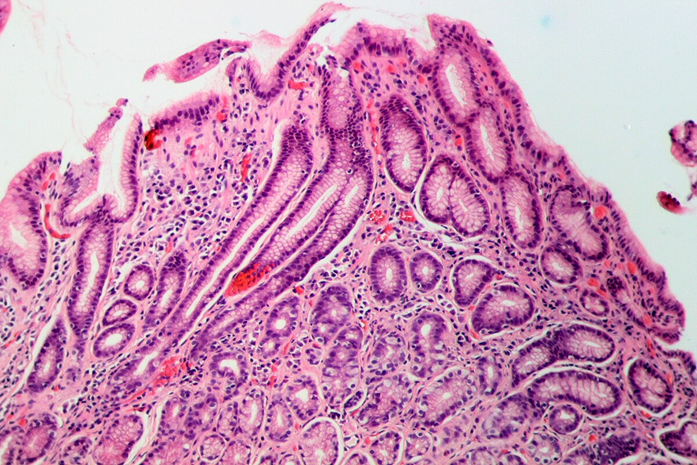
Chronic infection with Helicobacter pylori (H. pylori) is a well-established cause of serious upper gastrointestinal conditions, including peptic ulcers, gastric cancer, and MALT lymphoma. Eradicating H. pylori not only promotes ulcer healing and regression of gastric lymphomas but also significantly reduces the long-term risk of stomach cancer.
However, successful treatment depends on combination antibiotic therapy, most commonly involving clarithromycin, and its effectiveness is heavily influenced by local antibiotic resistance rates.
Current clinical guidelines advise against using clarithromycin-based regimens when resistance exceeds 15–20%, unless susceptibility testing is available. This is particularly relevant in Latin America, where H. pylori infection is widespread and gastric cancer remains one of the leading causes of cancer-related deaths.
Unfortunately, the region also faces a perfect storm of challenges: over-the-counter antibiotic access, frequent self-medication, and weak prescription controls, all of which contribute to rising rates of antibiotic-resistant H. pylori.
Table of Contents
A Literary Review to Understand Resistance Rates
Figure 2. Literary review. Source: Nuno Ribeiro via Flickr.
In a comprehensive systematic review published in The American Journal of Gastroenterology, Camargo et al. investigated the growing problem of Helicobacter pylori resistance to antibiotics in Latin America.
The study analyzed 59 observational studies conducted between 1988 and 2011, drawing data from across the region. Researchers focused on primary antibiotic resistance patterns in untreated adults, with a few studies including children and previously treated patients.
Using meta-analysis and meta-regression techniques, they assessed the prevalence of resistance to commonly used antibiotics in H. pylori eradication therapy. The findings revealed alarming resistance rates, particularly to metronidazole and clarithromycin, two antibiotics frequently used in first-line treatment.
On average, 53% of isolates were resistant to metronidazole, while 12% showed resistance to clarithromycin. These high rates seriously compromise the effectiveness of standard triple therapy, which typically combines a proton pump inhibitor (PPI) with amoxicillin and clarithromycin.
Antibiotic Resistance Varies by Antibiotic Regimen
Resistance to amoxicillin, tetracycline, and furazolidone, however, remained low, averaging 4%, 6%, and 3% respectively, making these antibiotics more reliable in Latin American treatment regimens. Resistance to fluoroquinolones like levofloxacin was also notable at around 15%, raising concerns for second-line therapy options.
Importantly, the study found no consistent trend in antibiotic resistance over time, indicating that resistance levels have remained persistently high rather than gradually increasing.
Only a small number of studies included pediatric populations, so data on antibiotic resistance in children remain limited. Additionally, including patients who had previously undergone eradication treatment did not significantly affect the overall resistance estimates.
A Call for Monitoring H. pylori Antibiotic Resistance
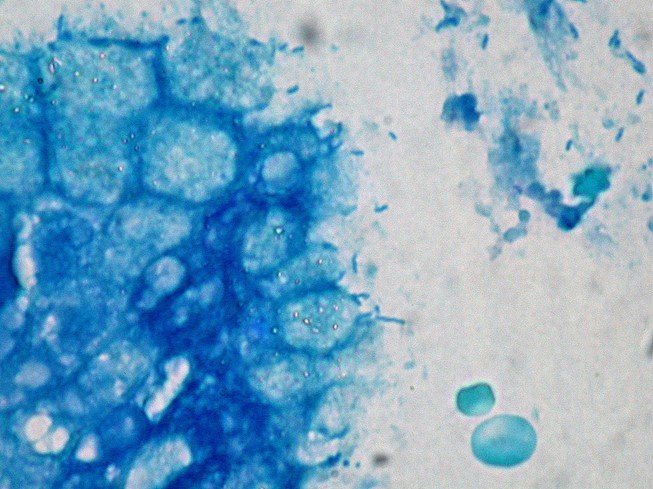
Figure 3. Helicobacter pylori in the gastric mucosa. Giemsa stain. Source: Ed Uthman via Flickr.
Beyond bacterial resistance, other factors such as smoking, poor medication adherence, and genetic variations affecting drug metabolism also reduce treatment efficacy. Few studies included pediatric populations, and most sampled urban, specialty-care populations, limiting generalizability to broader communities.
The authors urge national surveillance of H. pylori resistance, integrated with networks like ReLAVRA and WHONET. Better stewardship, public awareness, and region-specific treatment are key to reducing H. pylori-related diseases, especially gastric cancer, in Latin America.
The review also highlights that metronidazole resistance, while common, is less clinically impactful, as it can often be overcome by adding bismuth or extending treatment duration. However, increasing antibiotic use across Latin America, driven by self-medication, inadequate regulation, and rising retail sales, continues to fuel regional resistance trends.
In Summary
Ultimately, this review underscores the urgent need for regional antimicrobial surveillance, more judicious use of antibiotics, and updated clinical guidelines tailored to local resistance patterns.
With high clarithromycin and metronidazole resistance in Latin America, doctors should avoid empirical treatment. Regimens with amoxicillin, tetracycline, or furazolidone are more reliable. Boosting diagnostics and stewardship is key to controlling resistant H. pylori.