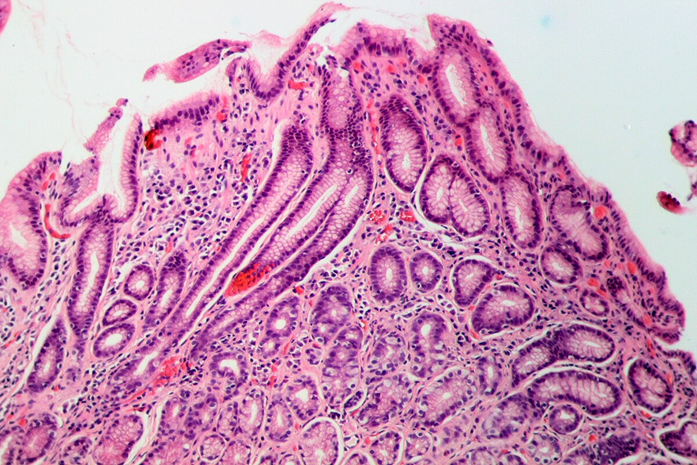
Gastritis due to H. pylori. Photo by Patho via Wikimedia Commons.
Highlights
- Multidrug resistance is common across Colombian H. pylori strains.
- Antibiotic resistance reflects underlying bacterial genetics.
- Key genetic mutations drive treatment failure.
- Genomic insights support precision treatment approaches.
- No association between antibiotic resistance and gastric cancer severity.
Multiple eradication regimens are in place for Helicobacter Pylori (H. pylori) in Latin America due to its high prevalence and oncogenic potential.
Standard first-line therapy, based on the Maastricht Consensus Report, typically includes a proton pump inhibitor (PPI) combined with two antibiotics, such as clarithromycin, metronidazole, or amoxicillin.
However, the rise of multidrug-resistant H. pylori has significantly reduced treatment success. Prior antibiotic exposure and widespread over-the-counter antibiotic use have fuelled antibiotic resistance.
Genetic Mutations Fueling Antibiotic Resistance
At the molecular level, resistance is linked to well-characterized genetic mutations, including:
- 23S rRNA mutations (A2142G/C, A2143G): clarithromycin resistance
- 16S rRNA mutations (AGA926–928TTC): tetracycline resistance
- gyrA QRDR mutations: fluoroquinolone resistance
- frxA/rdxA, rpoB (500–545), and pbp1A mutations: resistance to metronidazole, rifampin, and amoxicillin, respectively
Understanding these resistance mechanisms is essential for guiding precision-based treatment strategies and improving eradication outcomes.
In Colombia, for example, more than 85% of strains show resistance to metronidazole.
In this blog, we explore research by Mannion et al., published in the Journal of Clinical Microbiology, showing high levels of multidrug antibiotic resistance in H. pylori strains from Colombia, with implications for gastric cancer risk in different Colombian populations.
Methods for Investigating Antibiotic Resistance

Tumaco. Photo by El Tobias via Wikimedia Commons.
To map antibiotic resistance in Helicobacter pylori, researchers studied adults aged 40–60 with chronic digestive symptoms from two Colombian regions with sharply different gastric cancer risk: Túquerres, a high-risk area, and Tumaco, a low-risk area.
To avoid confounding results, participants had not taken antibiotics or acid-suppressing medications before undergoing endoscopy.
Gastric biopsy samples collected between 2006 and 2010 were analyzed using internationally accepted diagnostic standards, allowing researchers to evaluate both stomach tissue damage and bacterial growth.
H. Pylori Strains Identified
From these samples, 59 distinct H. pylori strains were successfully isolated.
These included 28 strains from a high-gastric-cancer-risk population in living in Túquerres and 31 strains from a low-gastric-cancer-risk population living in Tumaco.
Each strain was tested against six commonly prescribed antibiotics ( i.e., clarithromycin, amoxicillin, metronidazole, tetracycline, levofloxacin, and rifampin) using standardized laboratory methods recommended for clinical resistance testing.
To uncover why treatments fail at the genetic level, the team combined targeted gene sequencing with high-resolution whole-genome sequencing.
Key resistance-associated genes were analyzed alongside full genome structure and evolutionary relationships, revealing how genetic mutations and chromosomal changes shape antibiotic resistance across regions.
Genetic Mutations Driving H. pylori Resistance in Gastric Cancer Samples
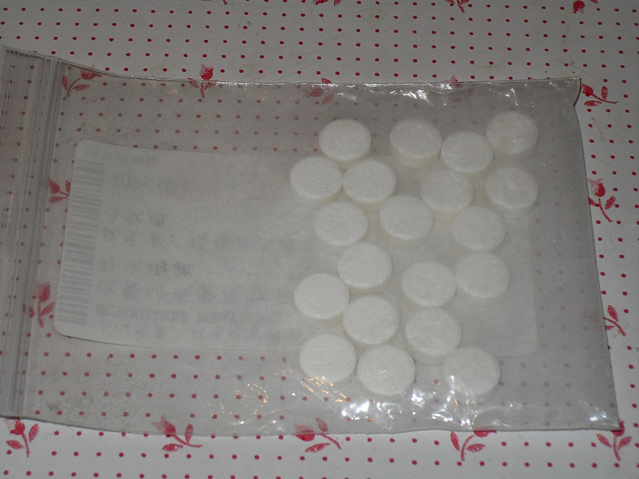
Metronidazole pills. Photo by Tomchiukc via Wikimedia Commons.
Some drugs worked well. Antibiotics like clarithromycin, amoxicillin, and rifampin remained effective because the bacteria had not altered the genes those drugs target.
Resistance to other antibiotics reflected specific genetic mutations. Most H. pylori isolates were resistant to metronidazole, while levofloxacin resistance was less frequent and tetracycline resistance remained rare.
Notably, metronidazole resistance was more prevalent in low–gastric cancer risk populations.
Mutations Against Levofloxacin
Levofloxacin, for example, targets a protein that H. pylori uses to copy its DNA. In about one out of every five infections, the bacteria carried small but critical mutations in a gene called gyrA.
These mutations subtly reshaped the target protein, preventing the antibiotic from binding. The result was predictable: when the mutation was present, the drug failed. When it wasn’t, the drug worked.
Mutations Against Metronidazole
Metronidazole told an even more revealing story. Unlike other antibiotics, this drug must be activated inside the bacterium to become lethal.
In most of the bacteria studied, the genes responsible for that activation, rdxA and frxA, were damaged, shortened, or completely broken.
Taken together, these findings change how treatment failure should be understood. In many cases, antibiotics fail not because of missed doses or reinfection, but because the bacterium has already rewritten the rules at the genetic level.
Why This Matters

Patient praying. Photo by Ahs856 via Wikimedia Commons.
Together, these findings show why one-size-fits-all treatment strategies fail. Antibiotics that work in one region may be ineffective just a few hundred kilometers away.
Without local resistance monitoring, doctors are often forced to guess, and patients could pay the price.
This has serious implications for Latin America. Clarithromycin and fluoroquinolones are widely used, not just for H. pylori but for respiratory and urinary infections.
This broad exposure increases the likelihood that resistance mutations arise long before gastric disease is diagnosed.
The study highlights a gap between scientific capability and clinical practice. While resistance mutations are detectable, they are rarely tested for, especially in resource-limited settings.
Stay Informed

Photo by DigiGal DZiner via Wikimedia Commons.
Understanding how microbial genetics shapes treatment failure is essential for improving patient outcomes.
Pathogenos provides evidence-based analysis of emerging infectious disease research, antibiotic resistance, and global health risks, translated clearly for real-world decision making.
Subscribe to receive updates on new findings, regional resistance trends, and research-driven insights that inform prevention and care.




